Where Are Mesenchymal Stem Cells Found?
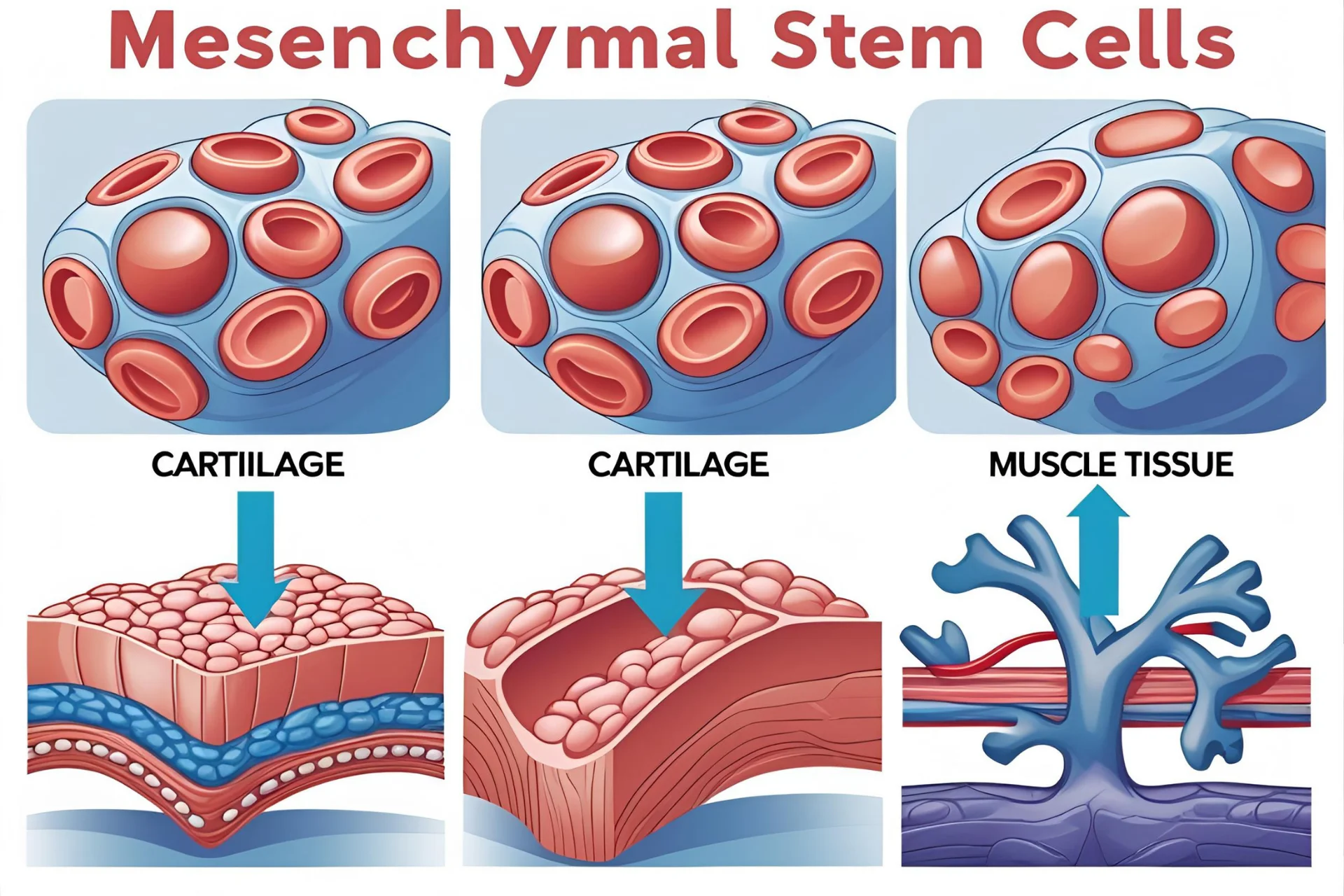
Mesenchymal Stem Cells (MSCs) are multipotent, self-renewing cells with the remarkable ability to differentiate into bone (osteoblasts), cartilage (chondrocytes), and fat cells (adipocytes). Known for their immunomodulatory and anti-inflammatory effects, MSCs are central to advancing modern regenerative medicine, cell-based therapy, and tissue engineering. Unlike embryonic stem cells, MSCs can be ethically sourced from various adult and perinatal tissues including bone marrow, adipose tissue, umbilical cord, and placenta. But where exactly are these regenerative powerhouses found—and how does the source impact their therapeutic potential?

What Are Mesenchymal Stem Cells (MSCs)?
Mesenchymal Stem Cells (MSCs) are a type of adult multipotent stem cell known for their ability to differentiate into various mesodermal lineages, such as bone, cartilage, and adipose tissue. Unlike pluripotent stem cells, MSCs do not form all tissue types but are highly valuable due to their self-renewal capacity and regenerative potential.
In the field of regenerative medicine, MSCs play a critical role by promoting tissue repair, reducing inflammation, and modulating immune responses. Their immunomodulatory properties make them especially promising for treating autoimmune diseases and inflammatory conditions.
The International Society for Cellular Therapy (ISCT) has established specific surface markers to identify human MSCs: CD105, CD73, and CD90 must be expressed, while hematopoietic markers like CD45 and CD34 should be absent. These markers help standardize MSC isolation and quality for both research and therapeutic use.
MSCs are now widely used in MSC-based therapies, stem cell transplantation, and emerging applications in personalized medicine, including tissue engineering and exosome-based treatments.
Primary Sources of Mesenchymal Stem Cells
MSCs can be isolated from several adult and perinatal tissues, each offering distinct biological characteristics, extraction methods, and therapeutic value. Understanding these primary sources helps researchers and clinicians select the most suitable MSC type for specific regenerative applications. The choice often depends on factors like cell yield, donor age, ethical considerations, and self-renewal potential.
Bone Marrow-Derived MSCs (BM-MSCs)
Bone marrow was the first tissue identified as a viable source of mesenchymal stem cells, making BM-MSCs the most studied subtype. Harvesting typically involves bone marrow aspiration, an invasive procedure usually performed under anesthesia. While the MSC yield from bone marrow is moderate compared to other sources, BM-MSCs have a long-standing record in stem cell transplantation and are often co-isolated with hematopoietic stem cells. These cells are widely used in orthopedic and hematologic therapies due to their well-characterized behavior.
Adipose-Derived MSCs (ADSCs)
Adipose tissue has emerged as a popular alternative for MSC collection, thanks to its high MSC yield and minimally invasive harvesting through liposuction. Known as ADSCs, these fat-derived stem cells are abundant and easy to isolate, making them ideal for large-scale regenerative therapies. ADSCs are commonly applied in cosmetic procedures, orthopedic treatments, and wound healing due to their robust regenerative profile and accessibility.
Umbilical Cord-Derived MSCs (UC-MSCs)
Collected immediately after birth, UC-MSCs are isolated from Wharton’s Jelly or umbilical cord blood. These neonatal MSCs are prized for their high proliferation rates and low immunogenicity, making them excellent candidates for allogeneic stem cell therapies. Unlike adult tissue sources, umbilical cord MSCs are obtained non-invasively and are considered ethically sound. They are increasingly used in pediatric regenerative therapies, immunological disorders, and stem cell banking.
Immunological disorders, and stem cell banking.
Placental and Amniotic Fluid MSCs
The placenta and amniotic fluid, typically discarded after childbirth, are rich in perinatal stem cells. These MSCs are considered less mature but offer a wide range of differentiation capabilities. Their collection is non-invasive and raises fewer ethical concerns, making them suitable for prenatal research, exosome-based therapy, and future cell-free therapeutic platforms. Despite being a relatively newer area of focus, placental MSCs show immense potential for regenerative and immunological applications.
Together, these sources demonstrate the flexibility and accessibility of mesenchymal stem cells across various tissues. Whether derived from adult fat, bone marrow, or perinatal structures like the umbilical cord and placenta, MSCs continue to shape the future of personalized medicine and regenerative therapies. Each source offers unique advantages, and ongoing research aims to standardize isolation methods for safer and more effective clinical applications.
Emerging and Niche Sources of MSCs
While bone marrow, adipose tissue, and umbilical cord remain the most widely used sources of mesenchymal stem cells, researchers continue to identify and explore alternative tissues that offer promising regenerative properties. These emerging sources may not yet be mainstream, but their unique biological characteristics and accessibility are opening new avenues in clinical research and personalized stem cell therapies.
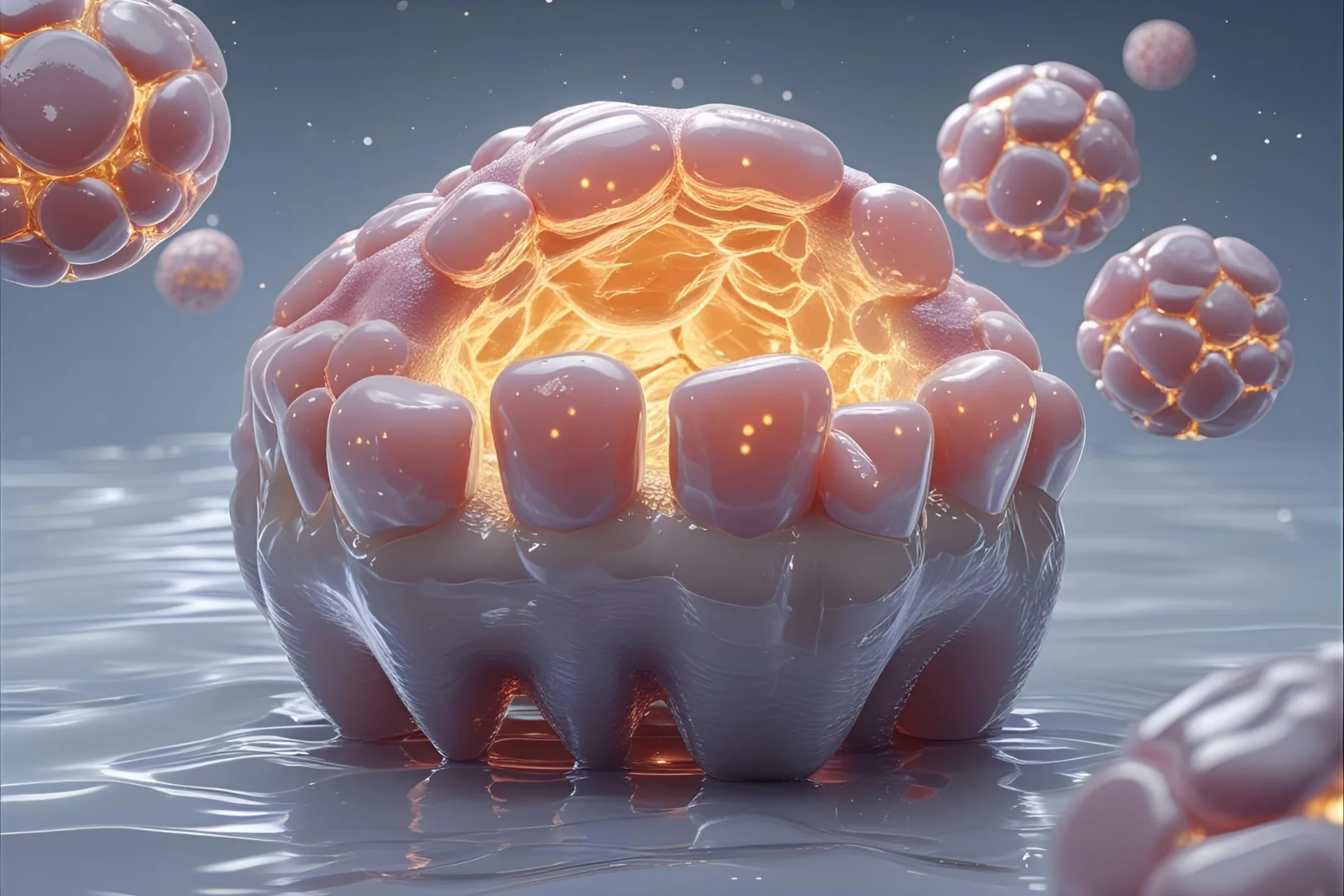
Dental Pulp Stem Cells (DPSCs
Dental pulp MSCs are isolated from the soft tissue inside baby teeth, wisdom teeth, or extracted molars. These stem cells from teeth can be collected during routine dental procedures, making them an accessible and minimally invasive source. DPSCs exhibit strong neurogenic potential, making them especially valuable in neuroregenerative research, craniofacial reconstruction, and maxillofacial surgery. As an emerging MSC source, DPSCs are also being studied for their role in treating neurological conditions such as Parkinson’s disease and spinal cord injuries.
Synovial Membrane and Peripheral Blood MSCs
The synovial membrane, found in joint linings, contains MSCs with exceptional potential for cartilage regeneration and joint repair, particularly in conditions like osteoarthritis. These synovial MSCs are being explored in orthopedic trials for their ability to support localized healing in damaged joints.
Peripheral blood MSCs, on the other hand, are rare and usually require stimulation through mobilizing agents to obtain a clinically useful quantity. While their extraction is less straightforward, these mobilized stem cells are of interest due to their ease of integration into circulating stem cell therapies and potential use in systemic conditions.
Comparison of MSC Sources: Yield, Access, and Application
Not all mesenchymal stem cell sources are equal. Each tissue offers a different balance of harvesting ease, cell yield, and therapeutic utility. Understanding these differences is crucial when selecting the most suitable MSC source for clinical or research purposes—whether the goal is autologous stem cell therapy (from the same individual) or allogeneic transplantation (from a donor).
Below is a comparison of the major MSC sources:
|
Source
|
Invasiveness
|
MSC Yield
|
Clinical Use |
|---|---|---|---|
|
Bone Marrow |
High |
Moderate |
High |
|
Adipose Tissue |
Low |
High |
High |
|
Umbilical Cord |
None |
Moderate |
Very High |
|
Placenta/Amniotic |
None |
Moderate |
Growing |
|
Dental Pulp |
Low |
Moderate |
Emerging |
Note: “Clinical Use” reflects both current FDA-approved applications and research-stage therapies.
To ensure safety and consistency, MSCs used in therapy must meet strict standards set by regulatory bodies like the FDA, EMA, and the International Society for Cellular Therapy (ISCT). Stem cell processing and storage should occur in GMP-compliant laboratories, ensuring the MSCs retain their immunomodulatory, proliferative, and multipotent characteristics.
Selecting between autologous and allogeneic MSCs also depends on treatment goals. Autologous cells are naturally compatible with the patient’s immune system but require an invasive harvest, while allogeneic MSCs, such as those derived from the umbilical cord or placenta, are more readily available and increasingly used in off-the-shelf stem cell products.
Below is a comparison of the major MSC sources:
Ethical and Regulatory Considerations
As mesenchymal stem cell (MSC) therapies gain traction, ethical sourcing and regulatory oversight are critical to ensuring safe and responsible use.
A major distinction exists between autologous and allogeneic MSCs:
These ethical stem cell sources, especially perinatal tissues discarded after birth, pose no harm to donors and avoid the controversies associated with embryonic cells.
Regulatory bodies such as the FDA, EMA, and ISCT set standards for MSC identity, manufacturing, and clinical use. Stem cells must be processed in GMP-compliant laboratories, ensuring consistency, sterility, and safety.
Institutions offering stem cell banking must also follow strict regulatory approval guidelines to store MSCs for future clinical or personal therapeutic use.